| ABOUT THE AUTHOR: James M. Swinehart, M.D. is a board certified dermatologic surgeon. He has practiced his specialty in Denver, Colorado for the past 18 years near Porter and Swedish Hospitals. |
James M. Swinehart, M.D. |
WHY A DERMATOLOGIC COSMETIC SURGERY NEWSLETTER? As physician and patient awareness of personal enhancement techniques has skyrocketed, surgical procedures have been perfected to meet this demand. Dermatologic surgeons have pioneered tumescent liposuction, hair transplant micrograft megasessions, chemical peels, dermabrasions, laser therapy, botox injection, dermal grafting, MOHS surgery, and many other techniques for surgery and therapy of skin disease. It is my hope that you will find this periodical enlightening and stimulating. |
TUMESCENT LIPOSUCTION |
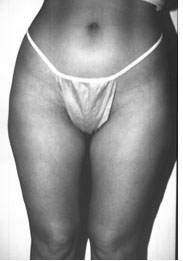
Patient in early 30's with excess fat on inner thighs, knees, and saddle bags. She could not lose this fat in spite of vigorous exercise. |
Beautiful results one month later from tumescent liposculpture. |
Liposuction in the modern era was first performed by Georgio Fischer, an Italian gynecologist, in 1976. The technique was subsequently exported to France by Yves Gerard Illouz and then by Pierre Fournier, who described the pre-icing technique called "neocryoanesthesia". The procedure was then developed here in America in 1982-1984 by the cosmetic surgeons Michael Elam, B. Teimourian, Saul Asken, Larry Field, and others. However, the early operative techniques were certainly not without problems. The old "dry technique", performed under general anesthesia without any local anesthesia, seemed to often produce "nothing but blood", limiting the amount of fat removal. The "wet technique", with spaced boluses of local anesthesia injected by syringe, produced only a slight decrease in bleeding. An article in the Journal of Plastic and Reconstructive Surgery in 1985 reported a complication rate of over 20%. In 1986, a group of complications in Houston made the national TV show "60 Minutes", greatly dampening the public enthusiasm for this procedure. A BREAKTHROUGH In response, Jeff Klein, a California dermatologic surgeon, invented the "tumescent technique" in 1985 and 1986, publishing his landmark paper in 1987 in the American Journal of Cosmetic Surgery. This technique was further highlighted when Dr. Klein was featured on "20/20" in both 1995 and 1996, in a positive vein. The purpose for this special program was that the producers of this nationwide news feature wished to make the public aware of the safety and efficacy of this dermatologist-developed technique. The show featured a patient speaking excitedly on a portable phone as she was undergoing liposuction by Dr. Klein. "Tumescence" is defined as "the condition or presence of swelling or enlargement" — in other words, expanding the tissues with fluid. The areas to be suctioned are infiltrated with dilute lidocaine (0.05%-0.1%), epinephrine (1 to 1,000,000), and sodium bicarbonate (10 milliequivalents per liter). When accomplished with care and finesse this mixture produces profound local anesthesia and hemostasis lasting over twelve hours. Tumescent anesthesia is also commonly utilized for dermabrasion, face lifting, hair transplantation, scalp lifting, and laser peels. Recent pharmacologic studies have shown that doses of up to 50 milligrams per kilogram are safe for tumescent liposuction, since the injected local anesthesia is absorbed over 12 to 24 hours from the body's fat compartments. Eighty percent of the injected local anesthetic is eventually absorbed, whereas only approximately 20% is either suctioned or drains post-operatively. In contrast to the older methods, the modern aspirate (which appears pure yellow to the eye) contains only 1% blood, with an average of 12 milliliters of blood per liter of aspirate. Therefore, the patient donates more blood for his or her preoperative lab work than during the actual procedure! In addition, lidocaine is bactericidal for many common skin pathogens, and the tumescent solution is thought to provide a good measure against surgical infection. When combined with sterile technique and preoperative antibiotics, the incidence of wound infection has decreased to nearly zero: the author has not encountered one infection in his personal practice, with hundreds of procedures performed over the past ten years! NEWER INSTRUMENTATION Today, the only remaining similarity of tumescent liposuction to the "old method" is that fat is removed through a tube. Long gone are the old "garden hose" 6 to 10 millimeter diameter suction cannulas and converted OB suction pumps. Today's state of the art equipment is quiet, sleek, and highly efficient. We lose approximately 1 millimeter of atmospheric pressure (mercury) for every 1,000 feet in altitude. Therefore, we can obtain a maximum suction vacuum pressure of 24 millimeters of mercury at 5,000 feet, versus 29 millimeters at sea level. The Reliance Company, based in Grand Junction, Colorado, has compensated for this fact by designing a highly efficient, extra quiet pump that operates well in the Rocky Mountains. It operates at such a whisper that quiet conversation between patient and staff, or soft music, may be heard easily even though the pump is kept only several feet away in the operating room. |
Automated Variable Speed Infusion Pump |
State of the Art Pump |
Microcannulas Utilized for Liposculpture |
For safety, patients are placed preoperatively on Duricef, which is started the day before surgery and continued for five days. We also utilize Hibiclens, as a body wash for two days preoperatively and on the morning of surgery. With this regimen, our clinic has not encountered one single infection in 10 years. Postoperative patients may take a Medrol six day dose pack to combat swelling if triamcinolone is not used in the intravenous solution. During the actual procedure, patients are monitored with pulse oximeter, cardiac monitor, and blood pressure monitor, with an intravenous line used continuously. A CRNA group is utilized if patients receive intravenous Versed, Fentanyl or Dipravan. A crash cart with defibrillator and emergency medications is always present and stocked in the surgical suite. The original Klein needle has also all but been replaced by motorized, variable-speed infusion devices. These small foot-switch pumps, operable from either side of the operating table, are attached to an IV bag containing the desired infiltration solution. The surgeon or anesthetist then utilizes a 16 gauge flexible multiport infusion cannula attached to this pump to rapidly administer the desired tumescent anesthesia. Infiltration should always be accomplished at a minimum of two levels. The deep fat compartments should be anesthetized first—one should feel the flexible blunt tip cruising against the fascia as the area is numbed. The very superficial fat is also infiltrated, providing a "peau d'orange" effect. Individuals with thicker fat pads should receive local anesthesia in the middle zones as well. All areas should be anesthetized (and suctioned) in crisscross fashion through a minimum of two incisions at, or close to, right angles to each other to achieve maximum uniformity and minimize "skip" areas. MICROCANNULAS The newest microcannulas (defined as those possessing an inside diameter of less than 2.5 millimeters) exemplify beautifully the application of Bernoulli's principal: the smaller the diameter of the tube, the faster the flow rate of the fluid through this tube (assuming that sufficient vacuum can be applied to effect this flow rate). The effective pump described above is certainly up to this task—subsequently, it was discovered the tumescent liposuction could be performed very effectively through cannulas as small as large- bore phlebotomy needles! By requiring less force, smaller cannulas improve accuracy in controlling the direction and depth of tunnels within the fat and enable one to place accurate tunnels at exact and different depths within the fat compartments. The coordinative use of a graduating sequence of microcannulas permits the removal of greater amounts of fat, with more uniform and smoother results, than could be achieved with larger cannulas. |
60 year old white male with excess fat in abdomen and chest |
Chest and abdomen are much flatter after tumescent liposculpture |
POSTOPERATIVE CARE Perioperative and postoperative care has also changed a great deal. The entire procedure is performed through tiny multiple incisions made with a #11 blade, as mentioned previously. All incisions are positioned so that each targeted area is suctioned from a minimum of two, and up to four, directions to ensure a uniform, even outcome. A recent paired comparison study was performed in San Diego with sutures placed on one side and no sutures on the other. Interestingly, the side without sutures healed with decreased scarring, presumably because of the lack of "stitch marks". Therefore, at the current time, most who perform this procedure do not place sutures except in cases where the patient may be traveling a substantial distance. |
53 year old female with protuberant abdomen and midriff |
Flat abdomen 2 weeks after procedure. Note thinner waist as well. |
Special disposable absorbent pads are then placed over each incision to remove the drainage over the next 24 to 48 hours. The drainage has the benefit of decreasing bruising and swelling in the postoperative period. These pads are covered with flexible, comfortable garments designed specifically for tumescent liposuction. Ideally, the garments are worn for several days postoperatively, affording an even contraction and collapse of the tunnels for a final uniform even result. These garments encourage direct contact of the floor and the roof of the tunnel, accelerating wound healing, hastening fibrosis, and speeding the disappearance of the tunnels. |
29 year old white female with unwanted buldges on saddle bags, lateral buttock region, inner thighs, and knees. |
Remarkable improvement is seen in all areas only two weeks post operatively from tumescent liposuction. |
NEXT ISSUE: Will the patient remain forever in a suspended state of blanched tumescence? How can the surgeon achieve bilaterally symmetrical, aesthetically pleasing results? How do we approach the various specific body areas? These, and other, exciting points will soon be brought to you in the issues to come. Dr. Swinehart specializes in Tumescent Liposculpture at 950 E. Harvard Avenue, #630, Denver, CO 80210 - Phone (303) 744-1202. Copyright 1997 CDC. |